The IDS-SR, IDS-C, QIDS-SR, and QIDS-C include items that rate the nine item symptom domains used to define a major depressive episode (APA 1994) (ICD-10). The IDS-SR and IDS-C include additional items to define melancholic and atypical symptom features, as well as their commonly associated symptoms (e.g. irritability, anxiety), and endogenous symptom features defined by the Research Diagnostic Criteria (RDC) (Spitzer et al. 1978).
To determine if the IDS-SR and IDS-C measure depression in a manner consistent with the most widely used assessments, Rush et al. (1996) examined the relationship between IDS and QIDS scores, and HRSD and BDI scores in a sample of 434 outpatients with major depressive disorder (MDD) and 103 normal controls. IDS and QIDS total scores were comparable to those obtained by the HRSD17 and BDI, with Pearson product moment correlations of 0.95 between the IDS-C and the HRSD, and 0.88 between the IDS-SR and the HRSD. The correlation coefficient between the IDS-C and IDS-SR was 0.91. The correlation between the BDI21 and the IDS-C was 0.86, while it was 0.93 between the BDI21 and the IDS-SR. The correlation between the BDI21 and the HRSD17 was 0.85. In a sample of 68 newly admitted inpatients with MDD Corruble et al. (1999) found the MADRS to be correlated with the IDS-C (c=0.81); and the 20-item depression factor from the SCL90 (Derogatis 1977) were correlated with the IDS-SR (c=0.84). Rush et al. (2004) found high correlations between the QIDS-SR, and the IDS-SR (c=0.96), HRSD17 (c=0.81), HRSD21 (c=0.82), and HRSD24 (c=0.84) at the exit interview after 12 weeks of acute phase outpatient treatment (n=596). Additionally, correlations between the IDS-SR and the HRSD17, HRSD21, HRSD24 total scores were 0.84, 0.85, and 0.86, respectively,providing evidence that the IDS and QIDS are measuring depressive symptoms in the same manner, Trivedi et al. (2004) found the QIDS-SR total score was highly correlated with the IDS-SR total score for 544 adult outpatients with MDD (c=0.83). They also found robust correlations between the QIDS-C and IDS-C total scores for outpatients with MDD (c=0.82, n=544) and Bipolar Disorder (BD) (c=0.81, n=402).
The IDS and QIDS are sensitive to changes in depressive severity in a manner consistent with the HRSD and BDI, with the IDS and QIDS demonstrating a greater sensitivity to change in the lower range of scores reported by 434 outpatients patients with MDD and 103 normal controls (Rush et al. 1996). In 68 newly admitted inpatients with a diagnosis of MDD, Corruble et al. (1999) found the IDS-C and IDS-SR to be as sensitive to change as the MADRS and the SCL90 (depression subscale). In 62 patients with MDD, Biggs et al. (2000) found the IDS-C and IDS-SR to be significantly more sensitive to detecting change than standard five item visual analogue physician and patient self-report global rating scales. In a retrospective analysis, Rush et al. (2000) found comparable levels of sensitivity to change in depressive severity when comparing HRSD24 and the IDS-SR scores in a sample of 993 outpatients with MDD. In 596 adult outpatients with chronic, nonpsychotic MDD, Rush et al. (2003) found the IDS-SR and QIDS-SR were equally sensitive to symptom change, when viewed as a discontinuous variable (response or remission), although the QIDS-SR seemed to be slightly less sensitive to residual symptoms that the longer IDS-SR. In 544 outpatients with MDD, and 402 outpatients with Bipolar Disorder (BP), Trivedi et al. (2004) reported finding equal sensitivity to symptom change when comparing the IDS-C, IDS-SR, QIDS-C, QIDS-SR, indicating high concurrent validity for all four scales. High concurrent validity was also documented based on the Medical Outcomes Study 12-item Short Form (SF-12) (Ware et al. 1996) mental health summary score for the population divided in quintiles based on their IDS and QIDS score. In 681 patients with chronic MDD assigned to 3 treatment groups (medication alone, medication and psychotherapy, psychotherapy alone), Rush et al. (2005) compared the HRSD24 and the IDS-SR and QIDS-SR ratings, finding comparable change scores within groups (the IDS-SR and QIDS-SR also confirmed response and remission rates based on the HRSD24).
The IDS and QIDS have been used to distinguish response from remission (Rush et al. 1996, 2000, 2003, 2004, 2005, Biggs et al. 2000, Trivedi et al. 2004), as well as to quantify between group treatment effects in open label and randomized controlled trials (Rush et al. 1996, 2000, 2003, 2005, Biggs et al. 2000, Trivedi et al. 2001, 2004, Corruble et al. 1999). The IDS30 assessments have demonstrated sensitivity and specificity equal to or in excess of the HRSD17 (Rush et al. 1996, 2000, 2003, in press), BDI (Rush et al. 1996), MADRS and SCL90 (Corruble et al. 1999), with the IDS assessments showing a slight advantage in the lower scoring ranges (Rush et al. 1996, Corruble et al. 1999).
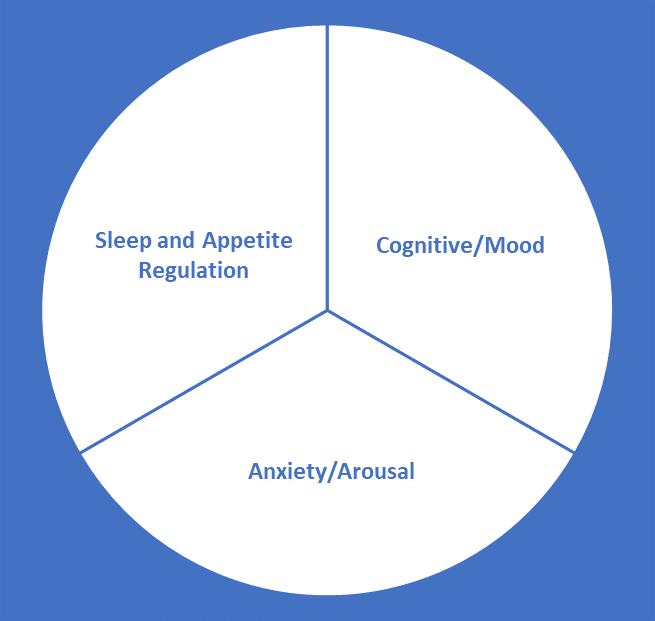
In 353 depressed outpatients, Rush et al. (1996) found three factors, 1) cognitive / mood, 2) anxiety / arousal, and 3) sleep and appetite regulation. However, the IDS is sufficiently unifactorial to allow for IRT analyses, and to create conversion tables with other standard ratings (Rush et al. 2003). Gullion and Rush (1998) factor analyzed a sample of 324 adult outpatients with MDD, concluding that when comparing the IDS with the HRSD, and the BDI, the IDS provided more complete coverage of the symptom constructs defined by the factor structure of the combined assessment items (Gullion and Rush 1998).
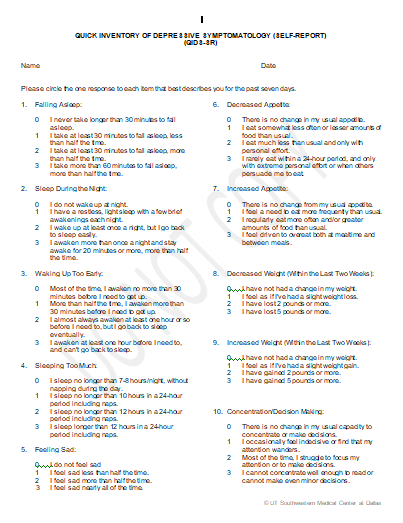
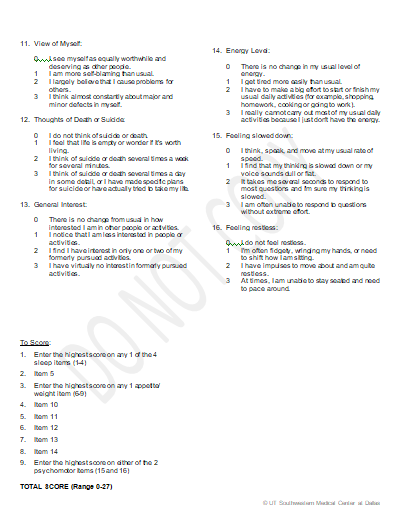
Note that the IDS30 contains all of the QIDS16 items, as well as mood reactivity, distinct mood quality, diurnal mood variation, irritable mood, anxious mood, capacity for pleasure, sexual interest, bodily aches and pains, panic or phobic symptoms, digestive problems, interpersonal rejection sensitivity, and leaden paralysis (Rush et al 1996). Both the IDS30 and QIDS16 rate symptoms for the prior 7 days (independent of whether they have been chronic, long-standing, or recent).