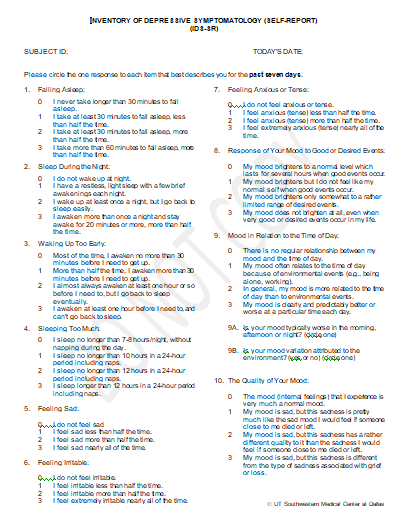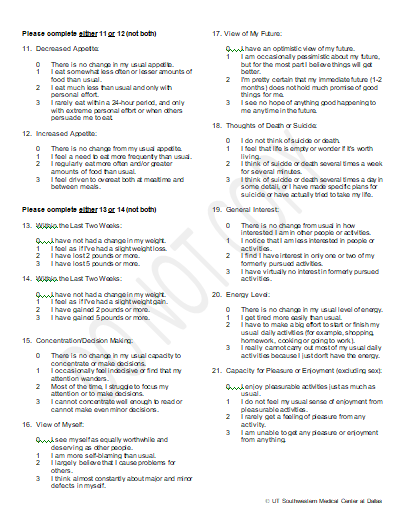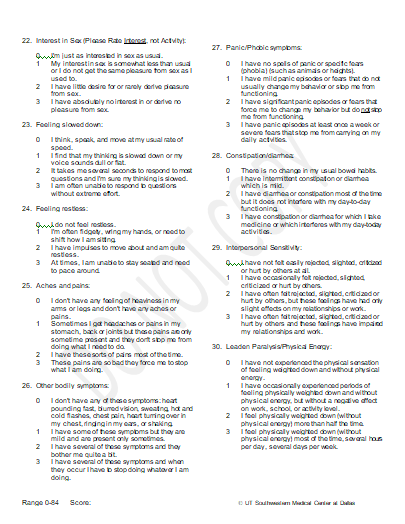
The 30 item Inventory of Depressive Symptomatology (IDS) (Rush et al. 1986, 1996) and the 16-item Quick Inventory of Depressive Symptomatology (QIDS) (Rush et al. 2003) are designed to assess the severity of depressive symptoms. Both the IDS and the QIDS are available in the clinician (IDS-C and QIDS-C) and self-rated versions (IDS-SR and QIDS-SR). Both he IDS and QIDS assess all the criterion symptom domains designated by the American Psychiatry Association Diagnostic and Statistical Manual of Mental Disorders - 4th edition (DSM-IV) (APA 1994) and the 5th edition add reference to diagnose a major depressive episode. These assessments can be also used to screen for depression, although they have been used predominantly as measures of symptom severity. The seven-day period prior to assessment is the usual time frame for assessing symptom severity.
The QIDS-C and QIDS-SR ask 16 questions by which to assess the severity of the nine diagnostic symptom criteria used in DSM. These nine criterion symptoms do not assess anxious, atypical, or melancholic features or other commonly associated symptoms such as pain or gastrointestinal disturbances. All 16 items (questions) on the QIDS are included within the IDS. The IDS-C and IDS-SR include the criterion symptoms, as well as commonly associated symptoms (e.g. anxiety, irritability) and items relevant to melancholic, or atypical symptom features.
Both the IDS and QIDS are easy to administer in either the clinician-rated (IDS-C and QIDS-C) or patient self-report (IDS-SR and QIDS-SR) versions; they require minimal training. Both versions are sensitive to change, with medications, psychotherapy, or somatic treatments, making them useful for both research and clinical purposes. The psychometric properties of both the IDS and QIDS, have both been established in various study samples.
There are several accepted clinician-rated and patient self-report measures of depressive symptoms. The most commonly used clinician rated scales are the 17, 21, 24, 28, and 31 item versions of the Hamilton Rating Scale for Depression (HRSD) (Hamilton 1960, 1967), and the 10-item Montgomery-Asberg Scale (Montgomery and Asberg 1979). The most frequently used self-reports include the 13, and 21 item version of the Beck Depression Inventory (BDI) (Beck et al. 1961), the BDI-II (Beck et al. 1996), the Zung Depression Rating Scale (Zung 1965), the Carroll Rating Scale (CRS) (Carroll et al. 1981), and the Patient Health Questionnaire - 9 (PHQ-9) (Kroenke et al. 2001). The IDS and QIDS have been compared to several of these measures.
The IDS and QIDS were developed to improve on the available clinician and patient ratings by 1) providing equivalent weightings (0-3) for each symptom item; 2) providing clearly stated anchors that estimate the frequency and severity of symptoms; 3) including all DSM-V criterion items required to diagnose a major depressive episode; and 4) providing matched clinician and patient ratings (Rush et al. 1986, 1996, 2003, 2005, in press, Gullion and Rush 1998, Trivedi et al 2004).
The items on the self-report and clinician rated version of the IDS-C and IDS-SR rate identical symptoms with equivalent anchors, as do the items of the QIDS-C and QIDS-SR. The self-report versions, the IDS-SR and QIDS-SR were developed to be easy to use severity measures, providing a potentially more time efficient alternative to the IDS-C and QIDS-C in both clinical or research settings.
Evidence of acceptable psychometric properties of the IDS-C and IDS-SR in depressed outpatients (Rush et al. 1996, 2000, 2003, in press, Gullion and Rush 1998, Trivedi et al. 2004) and depressed inpatients (Corruble et al. 1999) is available. There is also a substantial correlation between total scores on the IDS-C, IDS-SR, and the HRSD17 (Rush et al 1986, 1996, Gullion and Rush 1998). The IDS ratings have been shown to differentiate endogenous from nonendogenous depressions (Rush et al. 1987, Domken et al. 1994), dysthymic disorder from major depressive disorder (Rush et al. 1987), depressed from nondepressed radiation oncology patients (Jenkins et al. 1998), and depressed from nondepressed cocaine-dependent jail inmates (Suris et al. 2001).
Following the development of the IDS-C and IDS-SR we decided to provide a shorter, time-efficient, 16-item version for use in clinical research and daily practice, that focuses only on the nine DSM-IV criterion symptom domains. The resulting scales are called the Quick Inventory of Depressive Symptomatology – Clinician Rating (QIDS-C) and the Quick Inventory of Depressive Symptomatology – Self Report (QIDS-SR). The QIDS ratings were constructed by selecting only items from the 30 item scales needed to assess the nine DSM-IV criterion diagnostic symptom domains. The scoring system of the QIDS converts responses to the 16 separate items into the nine DSM-IV symptom criterion domains. The nine domains comprise 1) sad mood; 2) concentration; 3) self-criticism; 4) suicidal ideation; 5) interest; 6) energy/fatigue; 7) sleep disturbance (initial, middle, and late insomnia or hypersomnia); 8) decrease or increase in appetite or weight; and 9) psychomotor agitation or retardation. The total score ranges from 0 to 27.
Note that the IDS contains all of the QIDS items, as well as mood reactivity, distinct mood quality, diurnal mood variation, irritable mood, anxious mood, capacity for pleasure, sexual interest, bodily aches and pains, panic or phobic symptoms, digestive problems, interpersonal rejection sensitivity, and leaden paralysis (Rush et al 1996). Both the IDS and QIDS rate symptoms for the prior 7 days (independent of whether they have been chronic, long-standing, or recent).